Cím: | Homelessness and tuberculosis |
Szerző: | Dávid Bea, Oross Jolán, Vecsei Miklós |
Sorozatcím: | |
A kiadás helye: | Budapest |
A kiadás éve: | 1998 |
Kiadó: | Soros Alapítvány |
Terjedelem: | |
Nyelv: | angol |
Tárgyszavak: | TBC, hajléktalanság, tuberkulózis, egészségügy |
Állomány: | |
Megjegyzés: |  |
Annotáció: | |
ISBN: | 963 904 913 1 |
ISSN: | |
Raktári jelzet: | E |
Bea Dávid - Jolán Oross - Miklós Vecsei
Homelessness and tuberculosis
Manuscript read by:
Dr Dezső Kozma
György Mezei
Mária Szurkos
Translated by:
Alan Campbell
Produced as part of the
Soros Foundation Health System Development Programme.
Bea Dávid - Jolán Oross - Miklós Vecsei
Soros Foundation 1998
ISBN: 963 9049 131
Homelessness and tuberculosis
Program coordinated by
the Hungarian Maltese Charity Service
Budapest Centre
With special support from
The Foundation for Better Lif
Project participants:
National Korány Tuberculosis and Pulmonology Institute
SOTE Pulmonology Clinic
Budapest District III, IV, VIII, XIII, and XIV Pulmonary
Care Institutes
National Public Health and Medical Officer Service
Budapest Social Services Centre and its Institutions
Oltalom Charity Society
RÉS Foundation
Foundation for Healthy Breathing
Nógrádgárdony County Pulmonological Sanatorium
St John's Hospital, Budapest
Tutor Foundation
Introduction
In 1989-90, when the homeless people first appeared in great numbers, it was recognised from the beginning that this mass of people would become the breeding ground for many diseases, including tuberculosis. The eminent professor of pulmonology and alcoholism, László Levendel, who right up until his death was doctor to those in the worst social condition, called the attention of the medical profession, social services and the public at large to the dangers associated with homelessness. "The warning is plain to see, from their sorry condition, the traumatisation of their personal development, the multiple damage to their health, their slipping to the bottom of the social pile. Homeless people are in a dangerous, indeed critical condition. Although the problem originates within society at large, the situation above all demands health care and medical intervention." 1László Levendel saw a close relationship between homelessness, alcoholic diseases and tuberculosis. Whereas among alcoholics the tuberculosis rate is about ten times average, among homeless people it may be as much as one hundred times. Subsequent studies found rates of tuberculosis infection somewhat less than this, but still many times that of the general population.
In this report, we discuss the relationship between homelessness and tuberculosis, using to some extent the findings of earlier studies, but mostly those derived from this programme, aimed at screening homeless people living in Budapest for lung disorders. The planning and execution phases of the programme are discussed in detail, as are the dilemmas which arose, the attempts to solve them, and possible ways forward for the programme, including its expansion. We present an analysis of what we learned from the "screening interviews" held with homeless people as part of the programme, and compare the data with findings of earlier research.
Background
The recurrence of tuberculosis across the world2
At the beginning of the nineteen-eighties, the World Health Organisation (WHO) and the International Union Against Tuberculosis (IUAT) forecast that by the end of the century, the occurrence of tuberculosis would be merely sporadic. In 1989-90, the WHO carried out a worldwide survey of tuberculosis and stated in its report that tuberculosis now threatens the lives of more people than HÍV. Apart from malaria, tuberculosis now claims more victims than any other infectious disease.
WHO estimates the number of people infected with tuberculosis as 1.7 billion. The number of new patients is around 8 million, of which 95 per cent live in the developing countries. In 1990, tuberculosis claimed 3 million casualties, more than at the nadir of the disease at the turn of the century, when it took 2.1 million lives. WHO forecasts that tuberculosis will cause the death of 3.5 million people in 2000, mostly in the developing countries, unless the present WHO strategy is applied on a broad basis.
The general cause of the disease is poverty, i.e. bad social and health care conditions, undernourishment, lack of medicines, and the rise in the number of people with HÍV. (Countries with high rates of AIDS, the incidence3 of tuberculosis has doubled or trebled in comparison with previous years. Estimates put the number of people who were suffering from either tuberculosis or AIDS in 1993 to be around 5 million. Among American homeless people infected with both tuberculosis and AIDS, twenty or thirty out of every hundred do not respond to treatment by the traditional drugs, which can raise the cost of medical treatment, which would otherwise not be very high, by a factor of up to thirty.)
In Western European countries, for every hundred thousand of the population, about 20 new tuberculosis patients are registered annually. (An exception to this is Portugal, where the figure is about 50, and in Sweden, Norway and Denmark, it is only 8-10.)
In Eastern Europe, the number of new patients per hundred thousand of population is about 50. WHO figures for 1994 put the Hungarian figure at 41. In Romania, Poland and the former Soviet countries the figure is somewhat higher, and in the Czech Republic, Slovakia, Bulgaria and Slovenia, somewhat lower.
The recurrence of tuberculosis in Hungary
In Hungary, the epidemiological situation of tuberculosis in the first half of this century was particularly severe. In 1910, tuberculosis took first position in the list of causes of death and third position in 1930, going down to tenth in 1960. At the turn of the century four hundred per hundred thousand population died of tuberculosis, after the Second World War one hundred, but in 1995 this rate was 6.16. At the beginning of the 1950s, 30-35,000 new tuberculosis patients were registered, of which more than 5000 were children. The great decline in the incidence of tuberculosis took place between during 1960s, 70s and 80s. In the 1990s, however, the number of tuberculosis sufferers has gradually been increasing again, chiefly among those in the active age groups. The number of registered and new tuberculosis patients are shown in the two tables below, drawn from Central Statistical Office data.
Numbers of registered tuberculosis patients4
| 1980 | 1990 | 1993 | 1994 | 1995 |
| 15548 | 11176 | 11404 | 11895 | 12190 |
Numbers of new tuberculosis patients of each sex5
 | 1980 | 1990 | 1993 | 1994 | 1995 |
| Men | 3566 | 2533 | 2908 | 2880 | 3011 |
| Women | 1846 | 1055 | 1301 | 1283 | 1328 |
| Total | 5412 | 3588 | 4209 | 4163 | 4339 |
The number of new tuberculosis patients per ten thousand of population was 3.50 in 1990, 4.10 and 1994 and 4.24 in
1995.
Essential to the fight against tuberculosis is to find the factors underlying the spread of the disease. Dr. Ottó Schweiger6 has identified four chief factors:
● Lack of, or deficiencies in, an anti-tuberculosis programme.
● Population effects. (In countries where tuberculosis is common and population increase is high, people are exposed to greater risk of infection. The age distribution of the population also affects the spread of tuberculosis. Where there is a rising proportion of the middle-aged and elderly, tuberculosis spreads faster.)
● The vulnerability of the population to tuberculosis. (Responsibility for the spread of tuberculosis is may be attributed to risk factors affecting resistance to the disease. These include people who have contracted tuberculosis in the past, those infected with HV, and even those with other chronic diseases, such as diabetes, alcoholism, etc., the number of which is constantly rising.)
● Socio-economic effects. (Besides connections between tuberculosis and economic situation, the author also mentioned TB-infection among immigrants, which has become a significant risk factor since the beginning of the 1990s.)
It is now a general view, shared by the author that the ageing of the Hungarian population has led to a worsening of its state of health. The socio-economic situation has also worsened. A new factor is the appearance of immigrant tuberculosis sufferers. In the meantime, the structure of health care in the country has also changed. In place of hospital-centred care, priority has been transferred to outpatient care based on local doctors. This has led to an undermining of the pulmonary care system. In the opinion of the author, this would best be solved by modifying the former anti-tuberculosis programme in line with the changes, and directing anti-tuberculosis effort towards diagnosing tuberculosis infection and treating it as soon as possible.
Tuberculosis mortality7:
| 1948 | 1960 | 1970 | 1980 | 1985 | 1988 | 1990 | 1991 | 1992 | 1995 |
| 9972 | 3097 | 1991 | 1245 | 834 | 670 | 699 | 702 | 727 | 629 |
In 1995, 629 people died of TB
15-34 years 24
35-49 years 145
50-59 years 133
Over 60 327
Mortality per ten thousand of population: 6.16
Whereas in the past it was infants, children and those between 20 and 30 who were most stricken by tuberculosis, it is nowadays primarily a fatal disease for older men. Most of the deaths are among the over 60s, but this proportion is falling. Ten years ago only one in eight tuberculosis deaths were in the 35-49 age group, now it is one in five. The under-fifties accounted for 21 per cent of the 727 people who died of tuberculosis in 1992, and 27 per cent of the 629 deaths in 19958.
However, care must be taken in interpreting the tuberculosis mortality figures, because for a large proportion, tuberculosis was not the immediate cause of death. The tuberculosis mortality per ten thousand of population has changed from 1.2 in 1980 to 0.67 in 1990, 0.68 in 1993, 0.64 in 1994 and 0.61 in 1995, i.e. it has declined steadily.
Tuberculosis is nowadays a curable disease. Treatment of known TB patients is important for epidemiological as well as individual reasons. Where treatment is unsuccessful, the main reason is normally inadequate cooperation on the part of the patient (does not take medicines for sufficient time, takes them irregularly, etc.)9.
Lung screening in Hungary
A law of 1972 provided for lung screening examinations of the general public. It threatened summons, breach-of-regulations proceedings, and finally enforced treatment for tuberculosis patients who failed to meet their treatment obligations.
Act, Clause 31 (2) A person who is exposed to infection by, or to risk of contracting, tuberculosis, or who is suspected of having tuberculosis, or a person who has already been treated for tuberculosis in the past shall be obliged to subject him or herself to medical examination (care) on notification by the competent health care body.
GyR, Clause 31 (1) Any person who is found by lung screening or other medical examination to require medical examination for tuberculosis, any tuberculosis patient, any person exposed to tuberculosis infection, and any person who has already been treated for tuberculosis In the past shall be obliged, on notification by a doctor of the competent pulmonary treatment institution or by the doctor In charge of treatment, to present himself at the pulmonary treatment institution and subject himself to medical examination or treatment.
(3) If a tuberculosis patient does not present himself for medical examination or treatment despite the provision of paragraph (1), or drops out of treatment, then the pulmonary care institution's doctor, via the health visitor (nurse, district nurse), and subsequently by sealed registered letter, indicating the deadline and warning of the legal consequences (summons, misdemeanour proceedings), shall instruct him to present himself for medical examination or treatment at the pulmonary care institution. If the tuberculosis patient, despite written instruction by the pulmonary care institution, does not present himself for medical examination or treatment at the pulmonary care institution by the prescribed date, then the director of the institution shall contact the locally competent police force, in Budapest the district police force, to request summonsing of the patient for the purpose of medical examination or treatment. Consent of the public prosecutor shall not be required for implementation of the summons.
(4) If the tuberculosis patient does not abide by the health regulations, then the pulmonary care institution's doctor, via the health visitor (nurse, district nurse), and subsequently by sealed registered letter, indicating the deadline and warning of the legal consequences, shall instruct him to abide by the health regulations.
(5) If the tuberculosis patient still does not have himself treated after the enforcement measures mentioned in paragraph (3) have been implemented, or does not abide by the health regulations despite written warning, and by virtue of this behaviour puts at risk people in his immediate environment, then on the recommendation of the director of the pulmonary care institution, the State Public Health and Medical Officer Service may prescribe his placement in hospital. The patient may normally be referred to a hospital ward for three days. This period may, at the recommendation of the director of the hospital, be extended by the State Public Health and Medical Officer Service for three to six months. If the patient does not satisfy the terms of the referral, then the first level health authority may act in accordance with the provisions of paragraph (4) to summons the patient for the purpose of his placement in hospital.
(Extract from Act II of 1972)
In the past, members of the public were obliged on pain of fine to attend lung screening, but now there is no sanction for failure to attend. The Hungarian public is no longer afraid of tuberculosis and does not attend screening. Twenty years ago, some 7 million people attended lung screenings, but the corresponding figure for 1995 is only 4.2 million, in Budapest, only 60 per cent of the adult population take part in screening, and the people left out include precisely those most at risk.
A model investigation under way in Budapest10 found the highest rates of non-attendance at lung screenings in the district studied (Kőbánya) among the socially most at risk strata (eg. the temporary population - residents of workers' hostels, homeless people's hostels, old peoples' homes, etc.) and it was from these groups that patients suffering from rapidly-progressing, severe lung tuberculosis later emerged. The study found that in the district's temporary population (12-15,000 people), 72 people contracted TB between 1981 and 1993, and of these, 53 per cent had had no previous lung X-ray. This proportion is considerably higher than that among the permanent population, where only 8 per cent of patients had no previous lung X-ray.
Number of lung screenings, thousand people
| 1938 | 1950 | 1960 | 1970 | 1980 | 1990 | 1992 | 1993 | 1994 | 1995 |
| 269 | 2560 | 6448 | 7366 | 6480 | 4828 | 4720 | 4492 | 4418 | 4226 |
The numbers of people referred for further examination subsequent to screening were 238,000 in 1980, 169,000 in 1990 and 157,000 in 1995. The 1995 figure was 3.7 per cent of those screened.
Lung screenings in 1995 among Hungarian population
Screened 4.226.000
Referred 157.000
3,7%
among homeless people
Screened 2147
Referred 130
6%
We found that of the homeless people reached by our screening programme in 1995-96, 6 per cent had to be referred for further examination.
Risk groups
Instead of X-ray screening of the entire population, experts nowadays consider screening of risk groups to be the proper and efficient method. It is, however, far more difficult to carry out. Identification and registration of the members of risk groups demands considerable organisation. These special groups of the population are not always willing participants in screening, and so greater information and persuasion is necessary.
High-risk persons from a tuberculosis standpoint are all those for whom infectious TB has occurred in their family or surroundings, those who suffer from other risk diseases (eg. diabetes, silicosis, severe kidney disease, etc.) or chronic coughing.
High-risk groups include alcoholics and drug addicts, residents of various closed institutions or care institutions (eg. prisons, old people's homes, temporary accommodation centres, homeless refuges, etc.).
Old age, disadvantaged social situation, unsatisfactory living conditions and deficient nutrition also presents a source of TB infection risk.
The rate of TB infection among inmates of Hungarian prisons11 in 1990 was about five times the average in the public at large, and in 1994 it was more than 8 times the average. Nevertheless, there has been no screening in Budapest prisons since 1995. The main reason for this is that there is no mobile screening station in the city12
In Budapest prisons
1990
Inmates 13562
Tb patients 26
1994
Inmates 12846
TB patients 48
TB is a social disease
It is clear from the discussion of risk groups that tuberculosis is a serious threat to those living in bad social conditions. The rise in the incidence of lung TB, and the fatal course of the disease bear close relationships to social factors. We mentioned that the age distribution, decline in the state of health and economic situation of the population affect the number of people contracting TB, but a factor which must not be ignored is the ability of the health care structure to react to the changed circumstances.
In her book, Ártó-védő társadalom (The society that harms and protects) 13 writes that TB as a "social disease" has long been regarded as the "poverty disease", associated with the lower strata of society, with being poor and outcast. Sufferers are considered incurable, or more recently, incapable of healing. The author analyses the social characteristics of respiratory and other diseases (heart and vascular system, digestive, etc.). She identifies six life-aspect indices which determine the individual's social position, of which a composite index characterising material situation shows a stronger relation with respiratory diseases even than the "biosocial" indices (age and sex). It is standard of living, and especially wealth, that most consistently varies with occurrence of the disease. "... there is a disproportionate representation in the group of people with respiratory diseases of people whose bad relative material situation has not changed since childhood, so that they remain at the bottom of the social hierarchy." Of Ágnes Losonczi's sample, 4.6 per cent, chiefly middle-aged men living on the peripheries of society, had contracted TB at some time in their lives and had completely recovered.
Ágnes Bokor, in her book, "Poverty in Hungary today"14 , dedicated a separate chapter to the discussion of how poverty and deprivation is connected to the health-illness scale. Of the common diseases, mental and brain diseases occurred 4.4 times, and those of the circulatory system 3.6 times more frequently among deprived people. "Inequality is also a relatively high (2.6) in connection with infectious diseases, and urinary and reproductive organ diseases. Both are typical of the relation between traditional poverty and the distribution of diseases (primarily because of TB and the high number of births)."
Researchers in the 1990s have found that more than half of new TB patients live in disadvantaged conditions. Those most affected are alcoholics, drug addicts, the homeless and the unemployed. In Budapest, around 200 of the 900 new patients each year are homeless. Combined data from Budapest pulmonary care institutions show that there are more than one hundred active TB patients who have disappeared from view, most of them homeless.
An investigation carried out in the Korány Tuberculosis and Pulmonological Institute15 processed data of 27 patients who died of TB between 1 January 1990 and 30 June 1992. The social condition of the patients shows that nine of them lived alone, 16 of them suffered from alcoholism, one each was homeless and unemployed, and the living circum-stances of more than one-third of the patients (8) could not be established from their medical record card.
The authors of the study came to the conclusion that the victims were almost exclusively those with deviant lifestyles, and alcoholics, in whom TB was not detected at all or only so late that the extent of the disease and the bad condition of the patient was such that there was neither time nor opportunity to provide effective treatment. Alcoholism among people who contract tuberculosis is well known, but it is also striking that one-third of the patients were single and living alone. Presumably the same was true for those of unknown family background. About one-half of the patients also suffered from concurrent diseases, the treatment of which considerably increases hospital treatment time, and they had frequently been through many different wards before reaching the pulmonary ward.
In 1993, some 170 homeless people, or people deemed homeless, were treated in the SOTE Pulmonological Clinic16. Because of the lack of convalescent facilities, homeless patients had to be kept in hospital after the acute period, for humanitarian reasons, and this was accounted a major problem. On admission, the tuberculous patients were suffering from severe vitamin deficiencies caused by poverty and alcohol. Their incidental diseases were often of a severity commensurate with the primary diagnosis. A detailed personality study of 50 tuberculosis patients found that two-thirds did not have their own dwelling and were severely alcoholic. Their average age was 43.
Homeless people and tuberculosis17
Among homeless people in Budapest, compared with the general population, there is18:
twice the rate of persistent coughing persistent nervous problems insomnolence myocardial infarction poor hearing poor sight
three times the rate of choking complaints epilepsy
four times the rate of depressive conditions
five times the rate of limb fractures speech disorders
six-seven times the rate of attempted suicide
ten times the rate of tuberculosis
tfifteen times the incidence of parasites around twenty times the frequency of attendance at detoxification centres
Research into the health of homeless people both in Hungary and abroad has highlighted the high incidence of respiratory diseases, including tuberculosis. In Sweden, for example, TB was six times more common as a cause of death among homeless people than among the population as a whole.
In New York, a child health project showed that almost one-third of 3871 respiratory disease sufferers in the city hospital children's ward were homeless. There were twice as many respiratory illnesses among homeless children than among the child population as a whole. Of the 298 men and 230 women included in a study in Baltimore in 1989, 40 per cent of both sexes were suffering from respiratory diseases.
A British mortality study conducted in 1991 showed that the death rate among homeless people was 2.8 times higher than among the average population. Deaths from lung diseases in particular were three times more probable. 1991 data of the National Ambulatory Medical Care Survey (NACMS) showed that there are six times as many occurrences of respiratory diseases in the homeless population than the average.
And in Russia (St. Petersburg) a study of 600 homeless people was made in 1991. 55 per cent of those passing through screening were found to suffer from some respiratory or lung disease.
Data is also available on the state of health of homeless people in Hungary, In 1991, one of the first studies18 following the re-emergence of mass homelessness showed that 60 per cent of those questioned on admittance to a refuge had not attended lung screening for many years. The rate of lung diseases found on examination for various medical conditions was 11.5 per cent.
The first Hungarian research project on the state of health of homeless people to include a control sample took place in spring 199419. It found that the frequency of tuberculosis was ten times higher among homeless people than among the male controls in the city.
The Oltalom (Shelter) Hospital in Dankó Street in Budapest, set up for the treatment of homeless people, opened in February 1995. It admitted 446 patients in its first year of operation, of which 43 were fully-developed tuberculosis patients20.
A major contribution to the high rate of tuberculosis and lung diseases among homeless people comes from special risk factors arising from the homeless way of life: diagnostic uncertainties, difficulties of treatment and after-care, and the consequent danger of infection. Finding the patients (screening and bringing into treatment), treating them, and providing them with after-care, all demand a different approach from that applicable to the "resident" population, and a specially expanded set of facilities. The screening and treatment of homeless TB sufferers is a complex task, which can only be carried out effectively if there is close cooperation between health care and social services.
In view of the serious risks that homeless people are exposed to and the increased risk of infection arising from their way of life, workers in this field have for several years considered as one of their primary tasks lung screening of homeless people and organisation of treatment of the diseases thus diagnosed. This is partly implemented by requiring homeless people who are admitted to temporary accommodation to attend lung screening immediately or shortly afterwards. This, however, cannot be expected of people who use the night shelters which account for 30 per cent of the present accommodation system, daytime shelters, or meal services. These institutions are in principle obliged, if they operate satisfactorily, to accept those who demand their services on a "right to survive" basis, without referral, and the turnover of attenders is very high.
In his study of sleeping habits among homeless people coming into Budapest night shelters in 199521, György Mezei found that around one-half of homeless people in Budapest find a bed in a refuge. The time spent in refuges was rather short, but 5-10 per cent of those coming to refuges chose one night shelter as their "main place", and every seventh attender "moves about" between different refuges. This aggravates the problem of finding and screening sick, perhaps tuberculous homeless people. There is even more of a need for special methods to track down those homeless people who do not use places providing accommodation, but stay in hovels, caves, staircases, cellars, etc.
The lung screening programme for home less people
Preparations for the screening programme
In 1995, the Soros Foundation, after conducting preliminary consultations with professionals involved in services to the homeless, put out an invitation to tender for the implementation of the lung-screening programme for homeless people. Many applications were received from both Budapest and other large towns, from both health and social service institutions.
Weighing up the available financial resources with the applications received, and with particular heed to the specific considerations of the homeless people's conditions, we recommended, instead of individual judgement of applications which would have led to the funding of several isolated and projects of dubious effectiveness, the setting up of a pilot scheme to take place in Budapest with the close and coordinated cooperation of social service and health care organisations.
Meetings held with the applicants to discuss the proposal were successful. A joint decision was made to organise a comprehensive pilot screening programme in winter 1995-96 of the. Design of the programme called for adapting the screening, treatment and after-care stages to the peculiar demands of homeless people's mode of existence.
Issues to be addressed in planning of the Budapest homeless people lung screening programme:
Where should screening take place?
How should homeless people be sought out?
As stable sites where follow-up could also be pursued, the best candidates that emerged were those institutions for homeless people which provide services at a personal level, and various non-residential services. It was a fundamental precondition for the feasibility of the programme that it be capable of adapting to local conditions, and so the special features of candidate screening venues had to considered very carefully.
What were the sites considered for the screening programme?
Most of the homeless people who live in temporary hostels providing facilities for normal residence have to go through lung screening in the weeks following their admittance. A satisfactory routine has developed for tracking them and providing treatment. For this reason it is unnecessary to direct a special screening programme for the residents of temporary accommodation.
It is of vital importance, however, that there be balanced relations between the temporary hostels and the district pulmonary care centres and that screened patients be provided with treatment without difficulty.
The situation is different in the case of night shelters. These provide sleeping and washing facilities on a night-to-night basis, sometimes offering a modest dinner to people left on the Street and have no other accommodation open to them. Because of the way they operate, and the nature of their basic tasks, it is not possible for night shelters to tie their services to lung screening. Night shelters are mostly used by those in the worst condition even among homeless people -those least able to adapt, without income or work. Screening of people sleeping here was one of the programme's fundamental tasks. It demanded the involvement, and proper preparation, of social workers, and the motivation of the homeless people themselves.
One thing in favour of night-shelter screening was that all such places have "regulars". This allows large numbers of parallel screenings to be avoided. If necessary, people using night shelters could be reached by a "dispatch service" even if they were using various different refuges. Identification was made more difficult, however, by the fact that papers are not necessary for admission to night shelters, records mostly being made out on the basis of verbally-given details. Continuous attention also had to be given to the diagnosis and treatment of other diseases. There were well-known difficulties involved, but recourse could confidently be made to established practice in this field, to the homeless-people's ambulance service, and to the general practice surgeries and mobile medical services specifically set up to serve homeless people.
One candidate screening group is made up of clients of homeless people's social service offices, "people's offices", for the following reasons:
-a significant mass of Budapest homeless people are in contact with these offices,
-there are homeless people in contact with the offices who do not use any other institutional services - even night shelters,
-The offices continuously register those enquiring there -they have experience in organising appropriate medical care and providing social work services.
Homeless people who do not take up the services of other organisations can be reached in similarly large numbers in public bath facilities.
Baths are regularly attended especially by people who do not gain admission to any hostel. On the other hand, certification of disinfection is required in most hostels, and so those taking up hostel accommodation also appear at these places. One advantage was that the ÁNTSZ general practice surgeries for homeless people could be taken advantage of for treating other diseases and for arranging specialised care for patients.
A disadvantage was that tracking, identification and finding a second time seem to be practically insoluble, since there are no social workers employed either in the baths or the surgeries.
Other useful venues for screening are day shelters and soup kitchens. These facilities are "close to the streets" and many of their clients do not spend the night in hostels. Since there are few if any social workers operating in these institutions, and records and registration of clients are not incomplete, finding people a second time and providing follow-up after screening is also difficult here.
Homeless people who sleep on the streets and other places without coming near institutionalised services or health workers can only be contacted through Street social workers. Winter "tea rounds" stations are, like night shelters, ideal and effective locations for the screening programme. It is also the experience of mobile health services in recent years that they can reach people at these places, people left out of all institutional assistance, by following the "tea rounds".
In Street screenings, because of the high but essential incentives, there is a greater risk of duplication as well as problems of finding for a second time, so that accurate registration is most important.
Who and how?
Location, motivation, treatment, follow-up care.
In the screening places mentioned above, location of subjects is the task of social workers. In the case of street social workers, this is conceivably possible in conjunction with the "mobile doctors' surgeries", in parallel with treatment of various health problems and diseases, which for cases exceeding the facilities of mobile surgeries and homeless people's general practice surgeries, means the permanent involvement of ambulances and various treatment centres.
Motivation is served primarily by meeting the basic needs at an immediate level, promoting acceptance of screening examinations and possible treatment by the offer of hot tea, sandwiches, cigarettes, money, etc.
Screening examinations are partly X-rays carried out in pulmonary care centres and partly by bacteriological analysis of sputum. Where sputum samples are taken by social workers in daily contact with the homeless people at night shelters and other screening points, this work has to be pre-ceded by proper preparation. A mobile X-ray bus could also be brought into use alongside the sputum test. Second-time finding of screened people and motivating them to take part in treatment is a major task for the social workers or demands an effectively-operating "dispatch service" between the social and health centres.
Provision of treatment involves partly hospital and partly pulmonary care centre care, and provision of medicines. Among homeless people, health is not assigned a very high value, nor could it be, in view of the high risks of this mode of existence. In consequence, taking of medicines and regular medical control has little chance of being successful in an "outpatient" form, or at least such is only applicable to a very few of the people concerned.
Homeless people have no relatives and virtually no money, so that in order to make their treatment and stay in hospital go smoothly, medical care is not enough: continuous social work is needed to alleviate the isolation experienced in hospital, by regular visits and the provision of essential items like cleansing materials, underwear, extra food, social arrangements, etc.
This process then hands over to convalescence arrangements, which involve suitable temporary accommodation and good social work facilities. Danger of infection from patients can usually be eliminated after 6-8 weeks of hospital treatment. In order to effect final cure and prevent relapse, the patient may have to continue taking medicines for several months. Constant treatment of homeless TB patients can only be provided through an institution, which can keep constant relations with the patient and provide accommodation and meals. Here the patient receives medicines daily and in controlled circumstances. If this does not happen, then the disease will recur and the chances for treatment will be much poorer.
A screening programme for homeless people in Budapest, using the venues listed above and involving people with very special characteristics, and requiring a special set of approaches, is difficult to envisage as being run by only a health institution or only a social organisation. The complexity of the task is such that it is only achievable via the coordinated work of several health and several social institutions. It is important that those involved in running the programme do those parts, which they are best at, i.e. social workers do social work and doctors medical work.
The elements of such a system made up of social and health services were all present in the applications received in response to the programme announced by the Soros Foundation.
For the screening, treatment and after-care programme to be effective and clear to its participants, proper coordination is needed, a standalone task involving tying together the various strands, collecting and disseminating daily information, and keeping central records to allow future tracking. This is an essential service for programme participants.
Programme implementation
The first phase of the pilot programme proposed and financed by the Soros Foundation was coordinated by the Budapest Centre of Hungarian Maltese Charity Service, and took place between 1 December 1995 and 31 August 1996. The programme participants were five Budapest pulmonary care centres (Districts III, IV, VIII, XIII and XIV), the National Korányi TB and Pulmonological Institute, the SOTE Pulmonological Clinic, the Foundation for Clean Air, the Budapest Social Services Centre and its Institutions, and the RÉS Foundation.
Central to the success of the programme was the daily contact and dialogue which developed during the programme between the health and social service institutions and was the first of its kind (it unfortunately remains unique).
Under the programme, 3088 homeless people were contact-ed by 31 March 1996, mostly in night shelters, day shelters, free kitchens, public bathing facilities and in places suggested by the winter "tea rounds".
The programme was conducted in several stages.
First stage: making contact
The first task, making contact with the homeless people, was an exacting one for the social workers, involving several special problems. It was not enough to find homeless people in large numbers in the places they frequent. They also had to be won over to cooperation, homeless people not being known for enthusiasm towards prevention or early identification of disease. Another aspect was that the offer of money for taking part in a lung screening was likely to seem strange. Without it, however, it would have been very difficult to expect homeless people to wait in line, perhaps for several hours. In order to allay bad feelings, the homeless people were offered the payment (a packet of cigarettes) for completing a "screening interview", a short questionnaire. After completing the questionnaire, everybody was given a referral card to one of the district pulmonary care centres involved in the programme and a date for another appointment when they would be shown the result. The questionnaire, which bore all the deficiencies of short questionnaires, contained a few health questions giving the specialist doctors a basis to proceed on, and in the event that signs of TB were noted, a sputum sample was taken immediately, thus speeding up the detection process.
In a city where on average 42 per cent of men are smokers, the rate of smoking among homeless people is 90 per cent19
A word must be said about rewarding with cigarettes. It aroused deep emotions, and caused more dust to fly than the programme itself. Everybody felt that they had to speak up in defence of homeless people's health. We also received several letters and warnings from professional sources. Perhaps they were not aware of how much thought we had already put into this. The main reason was that we had about one hundred forints for the first reward (and less for the second). If we were to give out one hundred forints, it would firstly seem somewhat strange, and secondly involve much more administration, and time was a serious factor in this part of the programme. Beer, chocolate, cigarettes and canned food were the most likely suggestions. The majority opinion was, however, that cigarettes, which have the status of currency22 for homeless people, would be the most effective. Everybody knew, of course, that this would set off an anti-smoking battle, but a few facts won the argument: more than 90 per cent of homeless people smoke. Even if they do not want to, and even if they do not have their own cigarettes. They collect them most often at bus stops, and puffing on discarded cigarette-ends is a not inconsiderable source of infection. And in any case smoking is not banned in most hospitals, even in the pulmonary wards. One professor recounted, in consolation, a story of a young doctor in Germany in the 1960s who rented a bar, and every morning offered a glass of schnapps tó anyone who would take antituberculum. Many "disowned" him, but he cured a lot of people.
This story may seem rather long and beside the point, but it perhaps has a moral: it is not always possible to gain popularity points even with the most carefully-considered and professionally well thought-out procedures.
Second stage: screening
The great majority of homeless people attended the screening at the designated screening station, and most of them also came to the appointment which was usually set for the following week, where they were rewarded with a more substantial "motivation package". Unfortunately we were not spared mixed emotions on that occasion either, because we had to reward every person who had gone to the screening. (In the continuation of the programme, the screening bus will practically solve this dilemma.) Of course the week between screening and the second appointment did not pass completely uneventfully. Staff regularly went to the district pulmonary care centres for the results. We presumed that there would be some homeless people who would not be interested in the screening result and would not return to find it out, even for the sake of the motivation package. As it turned out, this was not in itself a bad thing, because some homeless people who went back for the results, on finding that they were infected, were struck with fear of hospital and isolation, and, because they as yet felt no pain, immediately absented themselves from the care centre.
People who were told at the second appointment that they were infected were usually more easily persuaded to accept hospital treatment. The hospital package (which also greatly helped the hospitals), the regular visits, and the fact that after discharge accommodation would be provided, was sufficient in most cases. However there was a problem with people who were ill but did not appear at the second appointment. These were searched for throughout the programme, with assistance from the homeless people's hostels in the city.
Another large and unforeseen problem was the matter of those referred to the pulmonary care centres. These were the people in whom lesions had been found, and although hospital treatment was not considered necessary, they should have attended the centres regularly. Unfortunately most were not prepared to do so, resulting in the worsening of their disease.
Of 3088 people, 2147 (70%) attended the screening.
1897 (61%) returned for the second appointment
941 people (30%) did not attend the screening
Off 2147screenings, 2017 had a negative result
130 people (6%) were referred for further examination
Of these, 50 were admitted to hospital. Two died in hospital.
Of the other 80 referrals, 4 seriously infected cases could not be found
76 people were prescribed further examination. Of these, 23 attended treatment regularly, but 53 could not be found.
How curable is tuberculosis?
Without suitable treatment, about 50% of tuberculosis patients die within 5-7 years. Patients who do not receive treatment present a serious risk infection to society. Sufferers diagnosed in good time can be reliably cured using available drugs. The World Health Organisation standard is a minimum recovery rate of 85% after first treatment, although this can be even better, up to 90%.
More than half of sufferers have to take 3 or 4 kinds of tablets for at least six months, and sometimes treatment is even longer. Treatment by injection is only used in certain more complicated cases. Regular medication is essential. Without it, the drugs become ineffective, and the bacteria become resistant to them. Recovery is drawn out or fails, and much more expensive treatment becomes necessary.
Surgical intervention nowadays is very rare, and consists of removal of one lung or one lung or lobe in a few per cent of cases if drug treatment is unsuccessful. The practice followed in Hungary is normally to treat new TB patients in hospital at least until they are no longer infectious, which takes around 6-8 weeks with suitable treatment.
Third stage: hospital treatment
During hospital treatment, the importance of flexible collaboration between social workers and health workers came to the fore. Although there were no tried and tested methods for many of the situations, this stage produced the fewest problems, and in fact the good working relations between different professions generated solutions to many other difficulties.
For example, the hospital indicated in advance to the after-care institutions how many beds would be required for convalescence, and so in most cases cured (i.e. non-infectious) patients could leave hospital immediately. These successes were also due to the programme's recognition that Hungarian health services at present are reluctant to deal with most homeless people. The reasons for this are the tendency for homeless patients' behaviour to breach norms, "cadging", or more often alcohol abuse and inability to pay. The former were addressed by frequent "relative-substitute" visits by social workers, and the latter by grants from the Soros Foundation.
Nevertheless, 4 people discharged themselves, and one was removed from hospital because of persistent alcohol consumption. The SOTE Pulmonological Clinic and the National Korányi TB and Pulmonological Institution treated a total of 78 homeless patients during the programme. 50 of these 78 were diagnosed through the screenings held by the programme. This 64 per cent screening rate far surpasses the 1995 national figure of 42 out of every 100 new patients being detected via screening.
Fourth stage: after-care
The availability of convalescent institutions was crucial to the success of the programme, because patients had to continue taking medication, and receive proper nutrition, for several months, in order to effect a complete recovery and to avoid recurrence. For people with no home, whose belongings are kept in a plastic bag, and who live irregularly, with no security, this is out of the question without assistance. Indeed without the after-care phase, the purpose of all the preceding operations would be called into doubt.
Of the 50 people hospitalised via the programme, 15 were transferred to other health institutions, and taking account of the 2 deaths, 4 self-discharges and l exclusion mentioned above, 28 required convalescent care.
Three entirely different kinds of institution were involved in this stage. One was a hospital ward (the "L" pavilion of the National Korányi TB and Pulmonological Institute) and two homeless people's institutions (Budapest Social Services Centre and Institutions, and the RÉS Foundation). The facilities in the homeless people's institutions were unfortunately very restricted, because their level of finance is much lower than that of hospitals. However, in these small-scale institutions, with their good separation, supervision and personal contact, prospects for recovery turned out to be better.
In the after-care stage, since with one exception the institutions were separate from the hospital, the involvement of district care centres was crucial. They provided the complete range of assistance throughout the programme.
At the time of reporting there are as yet no precise data on convalescence because of its duration. However, it is certain that the programme would have been unsuccessful without these kinds of institutions, backed up as they were by social work and rehabilitation support.
Summary
01 the 3088 homeless people reached by the 1995-96 pilot programme, 2147 (70 per cent) attended screening at one of the designated pulmonary care centres. 1897 people (61 per cent) returned for the second appointment to be certified as having attended screening. The care centres gave constant information on the results of screening. 2017 of the 2147 screenings were negative, and 130 (6 per cent) were referred for further examination. 50 of these 130 were admitted to hospital. (15 to the SOTE Pulmonological Clinic, 35 to the Korány TB and Pulmonological Institute.) Two of these 50 died in hospital. 28 were referred to convalescence facilities (FSZKI, RÉS Foundation, Korány TB and Pulmonological Institute). Some of those admitted for treatment were later reported to have discharged themselves from hospital or from the convalescent facilities.
Four of the people referred for further examination by screening -severely infected patients -disappeared and could not be found. The other 76 were referred for examination. Of these, 23 attended treatment regularly. We were unable to obtain information on the other 53 people. These were people referred by the care centres but not found to be infected or in need of hospital admission. Nevertheless, the irregularities discovered place them in the most at risk category. They may not be tuberculous, but may have broken ribs, or have suffered from pneumonia or similar trouble.
A total of 941 people (30 per cent) did not attend screening. Most of these live from casual work, or at least from occupations taking up some of the day (dustbin-raking, paper collection, bottle collection and return, begging). Part of the reason for their non-attendance may be that their time was taken up with the activities that bear them a living, or they may not have felt themselves to be ill, or they may have been unconcerned about the state of their own health. But these are the people in the worst condition. Although they did not turn up at the screening, many were later encountered in the pulmonary wards. They had been admitted via hospital wards, their tuberculous condition having been discovered after, for instance, road accidents or occurrence of other acute health problems, by which time their condition was usually serious.
The effectiveness of our screening programme is also shown by the fact that the detection rate of new patients from this mobile screening was some fifty per cent higher than that of traditional methods of screening.
The first mobile screenings
It was mentioned earlier that one of the greatest problems was carrying out the second appointment. Not only because many did not attend and finding infected patients demanded enormous extra work, but also because the "motivation package" was very costly.
The solution would have been a mobile screening station capable of producing immediate results, so that only one appointment would have been necessary. The programme was loaned a screening bus from the Nógrád County Council Pulmonological Institute in Nógrádgárdony, and we installed in it a darkroom and a film developer. Naturally the image quality fell far short of that of X-ray pictures taken in the district screening stations, but they were sufficient for picking out the serious cases and even more so for proving that progress can be made with this approach.
Between 3 and 7 June 1996, screening was held in 7 places using the bus borrowed from the Nógrádgárdony Pulmonological Institute. 50 of the further 494 homeless people had to be referred for examination, 11 required hospital treatment, two of which were new TB patients, and two disappeared before examinations were made.
The continuation of the programme
The efforts of the Soros Foundation and the Hungarian Maltese Charity Service have not been in vain. The programme is now drawing much more attention. The number of participants has also grown, and care has been widened by the incorporation of new elements. The Soros Foundation has continued to fund the programme. The social work accompanying the whole process is now carried out by the Tutor Foundation, set up expressly for the purpose. A new component of the programme is a rapid-test facility, provided by ÁNTSZ, to indicate in doubtful cases (when further examinations are necessary) the existence of TB within a few hours. These few hours, sometimes entire nights, have been undertaken by the Oltalom Charity Society, thus also ensuring vital professional medical support24. A new (!) state participant in convalescent care starting 1997 is the St. John's Hospital, Budapest. The most sensitive convalescence and rehabilitation cases are still taken by the RÉS Foundation. And most importantly: at the end of February 1997, the Hungarian Maltese Charity Service's new screening bus went into service, the gift of the "Foundation for Better Life". With its up-to-date equipment, it can produce excellent images within a few minutes. The running costs of the bus are being met in 1997 (and hopefully also in future) by the Ministry of Welfare.
Future hopes
The problem of the resurgence of tuberculosis is now clear, if not to everybody, certainly to the health profession. There have already been worthy attempts at addressing it (such as the Ajkay programme25 and the efforts of Dr. Anna Ungár26) but to tackle the problem at a level commensurate with its magnitude demands cohesion and convergence of objectives between civil organisations, and joint action by health and social services.
From our experience, it seems that of the 15-20,000 homeless people living in Budapest, 2 per cent can be regarded as TB sufferers in need of treatment - mostly infectious and constituting a high risk to their immediate and wider surroundings. Our mobile screening station can make a major contribution to discovering cases in good time, but setting up (or strengthening) the infrastructure for their treatment is an issue of vital urgency. Our programme has benefited from the work of many dedicated professionals, and continues to do so. However hospital facilities (sufficient hospital beds) to receive the patients, essential to arresting this disease, are as yet only partly available.
The programme continues, and we trust that the several hundred (!) tuberculosis sufferers wandering the streets of Budapest will get the treatment they need.
The picture emerging from the screening interviews
By virtue of the lung screening programme supported by the Soros Foundation, a large proportion of the most at-risk population of homeless people in Budapest has been reached for the first time, and tuberculosis and other serious diseases have been detected and treated. Screening took place in winter, in places frequented by homeless people who were otherwise unreachable by either social or health services. This is the only way by which they can be contacted, examined, and persuaded to take some care of their health.
The data
The basis of the data is largely the programme's "screening interview" which is made primarily for medical purposes (eg. to determine whether a sputum sample is necessary )27. Although these nearly 3000 questionnaires provide a significant database, some of the data from them must be treated with caution, and so the results must be regarded only as indicative. Since this is a population that hides from scrutiny, there is always some doubt surrounding the representativeness of the sample in any research into homeless people. The lessons learned have been used to tighten up and redraft the questionnaire used in the relaunched screening programme which started in December 1996.
Most of the data can be analysed both alone and in comparison with the results of similar research. Demographic variables were compared primarily with the results presented in Katalin Sarlós and György Mezei's study Nyomorskála (A Scale of Poverty)28, and data on state of health with László D. Molnár's 1994 study29 of the state of health of homeless people in Budapest.
These two studies highlighted the following two aspects: -in both cases the homeless people included in the sample were chosen - similarly to our own survey - at random, at several different places. In contrast to several other studies carried out in recent years30, therefore, it was not exclusively homeless people resident in hostels who were involved.
-The time that has elapsed between the other two surveys and the present one is relatively short.
As well as the whole sample (N = 2998), we compared two sub-samples with these two earlier studies. The sub-samples were distinguished on the basis of the tuberculosis screening results. The first and larger sample (N = 2906) is made up of those who only completed the questionnaire31 or whose diagnosis was negative. These will be referred to subsequently as the "healthy" group. The second sub-sample (N = 92)32 consisted of those screened positive. This sample includes those referred for both tuberculosis and other lung conditions. These are the "unhealthy" group.
A longer questionnaire was also completed by 78 tuberculosis patients referred to hospital by both the programme and by institutions for the homeless (the results of this are presented in Chapter 4).
Demographic data
Sex
The proportion of men in the whole sample was 91 per cent (2178 people), and of women, 9 per cent (278). Similar proportions were found in both the sub-samples.
Compared with a proportion of over 50 per cent in the Hungarian population as a whole, women only comprise between 9 and 22 per cent33 of samples in various studies of homeless people.
Age groups
Distribution of homeless people by sex
Table 1
 | 20-29 | 30-39 | 40-49 | 50-59 | 60< | Total |
Men
% | 273
10 | 640
24 | 1032
39 | 570
22 | 141
5 | 2656
100 |
Women
% | 33
12 | 63
23 | 111
41 | 48
18 | 16
6 | 271
100 |
Total
% | 306
10 | 703
24 | 1143
39 | 618
21 | 157
6 | 2927
100 |
Demographic data 1996 (in %)
Table 2
 | 20-29 | 30-39 | 40-49 | 50-59 | 60< | Total |
| Men | 22 | 19 | 22 | 17 | 20 | 100 |
| Women | 18 | 16 | 20 | 16 | 30 | 100 |
| Total | 20 | 17 | 21 | 16 | 26 | 100 |
These two tables show that the 30-59 age group account for 54 per cent of the total over-20 Hungarian population, but more than 80 per cent of the homeless people questioned during our lung screening programme. Ali of the earlier studies already mentioned concur that the overwhelming majority of homeless people are middle-aged (30-59 years old) and the proportion of old people in this population compared to that of Hungary as a whole is very small.
Comparison of age distribution found in different studies3
Table 3
 | Whole population | Soros | Mezei | D.Molnár |
| 20-29 | 20 | 10 | 15,5 | (18-39 years)
41 |
| 30-39 | 17 | 24 | 28 |  |
| 40-59 | 37 | 60 | 47,5 | 52 |
| 60> | 26 | 5 | 9 | 7 |
The "otherness" of homeless people in figures
Population34
Women 52%
30-59 years of age 54%
Manual workers 15%
Born in Budapest 19%
Homeless people35
Women 9%
30-59 years of age 84%
Manual workers 50%
Born in Budapest 34%
We did not find a difference between the sexes in terms of age group37. The average age of the entire sample was 43; 43 for men and 42 for women. (In the Mezei-Sarlós study the average age of homeless people was 43.9 years.)
Distribution by place of birth
We are aware that the distribution of the homeless population by place of birth does not by itself tell us much. And comparison of our figures with the whole population must also be treated with caution because of the lack of precise comparative data.
These figures were unfortunately not sufficient for us to establish the role of various structural causes (unemployment, decline in standard of living, fewer workers' hostels) and individual, personal, psychological causes (lack of adaptive capability) in a person's becoming homeless. We hope that the 1997 survey, in which we included the question of whether the person arrived in Budapest already homeless or became homeless in Budapest, will provide an answer to this intriguing question.
However there are some quite striking figures. 34 per cent of homeless people were born in Budapest38. This percentage seems very high in comparison with both the Mezei study (around 25 per cent) and the total population.
In table 4, the first column shows the distribution of homeless people form outside Budapest by place of birth. The second column shows the percentages of all migrants to Budapest from different counties of origin, and the third column the distribution of the total population now resident in these counties.
Table 4
 | 1 | 2 | 3 |
 | Place of birth of homeless people (%) | Starting point of migrants to Budapest39 (%) | Distribution of non-Budapest adult popul40 (%) |
| Selected counties |  |  |  |
| Borsod | 11 | 9 | 9 |
| Hajdú-Bihar | 7 | 4 | 6,5 |
| Jász-Nagykun-Szolnok | 8 | 5 | 5 |
| Szabolcs | 17 | 7 | 7 |
| Total East Hungary: | 64 | 42 | 50 |
| Total West Hungary | 26 | 27 | 38 |
| Pest county | 10 | 31 | 12 |
Compared with the population at large, the proportions of homeless people are higher from East Hungary and lower from West Hungary and Pest county. This can clearly be attributed to the worse economic circumstances and higher unemployment in the eastern counties. We picked out the four counties which appeared in the highest proportions among the places of birth of homeless people. Of these, Szabolcs-Szatmár county stands out in particular: the pro-portion of homeless people born here is considerably higher than in any other county. The more prosperous western counties are represented in smaller proportions, relative to their populations, among Budapest homeless people.
When people become homeless
The screening questionnaire also asked when the person when he or she had become homeless , i.e. since when they regarded themselves as homeless41. The responses must be treated with caution for several reasons. Firstly, the responses were not given as precise dates, and secondly the moment of becoming homeless cannot be defined exactly - some consider it to be the date of moving out of home, or cessation of permanent residence, others the cessation of lodgings or discharge from a workers' hostel, and still others the release from prison or the breakdown of a family relation-ship. It is also common for a homeless people living for an extended period in a temporary hostel not to regard himself as homeless from the date of moving into the hostel.
Time of becoming homeless, for each sex
Table 5
 | <1 month before | 6 months before | 1 year before | 2 years before | 3 years before | 4-6 years before | 7-10 years before | > 10 < years before | Total |
Men
% | 226
9 | 153
6 | 351
13 | 409
16 | 367
14 | 669
26 | 262
10 | 149
6 | 2586
100 |
Women
% | 36
15,1 | 20
8,4 | 44
18,4 | 39
16,3 | 40
16,7 | 45
18,8 | 12
5,0 | 3
1,3 | 239
100 |
Total
% | 262
9 | 173
6 | 395
14 | 448
16 | 407
14 | 714
25 | 274
10 | 152
6 | 2825
100 |
The average number of months spent homeless was 43.4 for the whole sample42, 44.4 for men and 32.5 for women. The proportion having become homeless within the previous year was high, and matches the results of four years ago, at around 30 per cent of respondents. Unfortunately there is no data concerning the reasons why the newly homeless became so.
The table also shows that the proportions of women and men vary significantly with the time of becoming homeless. 42 per cent of women became homeless within the preceding year, compared with only 28 per cent of men. Women made up 12 per cent of all people who had become homeless less than one year previously, and only 2 per cent of those who had been homeless for more than 10 years. These figures support the hypothesis that there are more women among newly homeless people.
Time of becoming homeless 1992
Within last year 28,9%
1-4 years 36,5%
over 4 years 34,6%
Average time 51 months
Men 54 months
Women 27 months
Source: Mezei-Sarlós (1995)
"Healthy" and "unhealthy" homeless people
Those homeless people whose screening was negative were termed "healthy" in further data processing, and those with positive results, "unhealthy".
Age distribution in the two sub-samples
Table 6
 | <19 | 20-29 | 30-39 | 40-49 | 50-59 | >60 | Total |
Healthy
% | 54
2 | 303
11 | 693
24 | 1099
38 | 590
20 | 154
5 | 2893
100 |
Unhealthy
% | 1
1 | 3
3 | 10
11 | 45
50 | 29
32 | 3
3 | 91
100 |
Total
% | 55
2 | 306
10 | 703
24 | 1144
38 | 619
21 | 157
5 | 2984
100 |
The age distribution of the two samples is different. 63 per cent of respondents in the "healthy" sub-sample were under 40, compared with 85 per cent in the "unhealthy" sample. The average age was 48 years in "healthy" group, 4 years higher than the overall population.
Time of becoming homeless in the two sub-samples
Table 7
 | <1 month before | 6 months before | 1 year before | 2 years before | 3 years before | 4-6 before years | 7-10 years before | > 10 years before | Total |
Healthy
% | 260
10 | 170
6 | 386
14 | 436
16 | 396
14 | 683
25 | 260
10 | 149
5 | 2740
100 |
Unhealthy
% | 3
3 | 3
3 | 9
10 | 12
14 | 11
12 | 32
37 | 14
16 | 3
3 | 87
100 |
Total
% | 263
9 | 173
6 | 395
14 | 448
16 | 407
15 | 715
25 | 274
10 | 152
5 | 2827
100 |
We did not find differences between the "healthy" and the "unhealthy" groups in respect of sex. There were striking differences, however, in respect of the length of time spent homeless: 40 per cent of the "healthy" sub-group had been homeless for more than 4 years compared with 56 per cent of the "unhealthy" sub-group.
The average time spent homeless was 43.1 months in the "healthy" and 51.6 months in the "unhealthy" groups. The harsh conditions among which those living on the street live wears down their resistance in time. Those who have been living without a home for long periods are severely weakened and become more seriously ill, have great difficulty recovering, and are more likely to relapse. 17 per cent of the "unhealthy" group had already been treated for TB, and 23 per cent also had other diseases (see later).
State of health and risk factors
The screening interview also included questions on health care, state of health and some risk factors (smoking and alcohol).
Table 8 presents the personal health-related questions and the distribution or responses in the two sub-samples.
Distribution of responses to health-related questions
(Number of yes responses and their percentage.)
Table 8
 | Have you already been treated for TB? | Do you have any other complaints? | Do you “another disease”? | Do you smoke? | Do you consume alcohol every day? | Do you feel healthy? |
Healthy
% | 86
3 | 452
18 | 408
14 | 2640
91 | 1612
56 | 2575
89 |
Unhealthy
% | 15
17 | 20
21 | 23
25 | 85
94 | 40
45 | 73
81 |
Men
% | 92
3 | 411
17 | 371
14 | 2486
92 | 1574
58 | 2409
90 |
Women
% | 9
3 | 61
25 | 60
22 | 237
86 | 76
27 | 237
86 |
Tot. sample
% | 101
3 | 472
18 | 431
14,5 | 2725
91 | 1652
55 | 2648
89 |
52.5 per cent of respondents had social security cards and were therefore entitled to health care. A positive answer to the question of whether they had had tuberculosis before was given by 3.3 per cent of respondents. This proportion was 17 per cent in the "unhealthy" group.
The highest rate of having been already treated for tuberculosis was found among those who had become homeless between 4-6 years previously (5 per cent), (in László D. Molnár's study, 4.3 per cent of the homeless men had been previously treated for tuberculosis or catarrh of the apex pulmonis.)
Of "unhealthy" homeless people, 25 per cent also complained of other diseases. The figure for the entire sample was 18 per cent. Nearly twice as many women mentioned different diseases (22 per cent) than men (14 per cent), (in László D. Molnár's survey, 44 per cent of homeless men and 26.5 per cent of the control group complained of more than one disease.)
89 per cent of the complete sample replied affirmatively to the question, "Do you feel healthy?" Considering the state of health of homeless people, this figure is truly surprising, but considering the homeless mode of existence, perhaps less so.
91 per cent of the complete sample smoked and 55 per cent consumed alcohol daily. Fewer of the women said that they smoked (86 per cent), and significantly fewer said they consumed alcohol (27 per cent), in the "unhealthy" sub-sample, more smoked than the average, but fewer said that they consumed alcohol daily.
74 per cent of the entire sample had been smoking for more than 10 years regardless of when they became homeless. The situation was somewhat different with alcohol consumption. The longer somebody had been on the street, the more likely it was that he consumed alcohol. Whereas one-quarter of homeless people who had only become so within the preceding year, 46 per cent of those who had been on the street for more than 10 years consumed alcohol regularly.
"Who can you get help from?"
The responses to be selected from for this question were institutions (organisations serving homeless people, local government, other institutional service) and individuals (parent, child, spouse, partner, relative, friend, acquaintance, colleague, social worker, other) to whom the respondents could turn to for help. It was found that many more of the respondents would approach institutions (63 per cent) than individuals (13 per cent). Women were much more likely to feel they could get help from individuals (22 per cent) than men (12 per cent).
Who do you go to for help?
(Numbers and percentages of yes responses)
Table 9
 | Institutions
(N=2821) | Persons
(N=2315) |
Healthy
% | 1728
63 | 295
13 |
Unhealthy
% | 60
69 | 10
13 |
Men
% | 1629
64 | 258
12 |
Women
% | 159
63 | 47
22 |
Entire sample
% | 1788
63 | 305
13 |
Those who said they turn to persons for help indicated the following persons:
Relative 32%
Acquaintance 21%
Friend 19%
Parent 8%
Social worker 8%
Spouse 4%
Child 3%
Other 3%
Colleague 2%
It seems that homeless people tend mostly to rely on relationships with relatives and those outside their own family. Social workers, professional helpers, came fifth on the list.
Interview venues
The screening programme was conducted in a total of twenty-two places. These were divided into three categories for the purposes of analysis, to examine whether there were differences by sex, state of health and age between people screened in different places. The "hostel" category was made up of various temporary hostel facilities, the "day shelter" category by soup kitchens and day shelters, and the third category consisted of various public spaces.
Distribution of screening subjects at the screening venues by sex and state of health.
Table 10
| Sub-samples screening venues | “day shelters” | “hostels” | “public places” | Total |
Men
% | 1346
50 | 744
27 | 628
23 | 2718
100 |
Women
% | 128
46 | 56
20 | 94
34 | 278
100 |
Total
% | 1474
49 | 800
27 | 722
24 | 2996
100 |
Healthy
% | 786
27 | 786
49 | 706
24 | 2278
100 |
Unhealthy
% | 61
67 | 15
16 | 16
17 | 92
100 |
Total
% | 847
36 | 801
34 | 722
30 | 2370
100 |
It is clear from the table that a significantly higher proportion of women spend their time in public places, which makes it extremely difficult to contact them and estimate their numbers. Significantly more of the "unhealthy" group were to be found in places offering daytime facilities.
For purposes of finding homeless women it is therefore important to carry out screening or any other investigation in public places, whereas sick people are more concentrated at day facilities.
Table 10 and the detailed results seem to confirm the hypothesis that the homeless population is not homogeneous. The various groups of homeless people are quite distinctive from each other in terms of places they frequent, and their age, state of health, etc. For screening or any other programme involving homeless people, it is essential to discover how the different groups of homeless people differ from each other, and how they are most easily contacted.
It has already been mentioned that there was a variation, by several parameters, in the composition of homeless people interviewed in different screening venues.
Distribution of some variables by screening venue
Table 11
| Variables (%) | "day shelters" | "hostels" | "public
places" | Entire sarnple |
| Positive diagnosis | 4 | 2 | 2 | 3 |
| Proportion of women | 9 | 7 | 13 | 9 |
| Age (average* years) | 44 | 44 | 43 | 43 |
| Time homeless (average months) | 44.5 | 42.5 | 42 | 43 |
| Born in Budapest | 32 | 33 | 36 | 33 |
| Do you feel healthy? (yes) | 91 | 85 | 90 | 89 |
| Other disease | 14 | 17 | 12 | 14 |
| Visited doctor in last month | 29 | 37 | 39 | 32 |
| Have you lost weight? (yes) | 36 | 33 | 26 | 33 |
| Asked help from organisation? (yes) | 73 | 61 | 48 | 63 |
| Asked help from person? (yes) | 16 | 10 | 13 | 13 |
The above table is clearly not sufficient to form a clear picture of homeless types. The screening venues are not exactly the same as the places where respondents spend their days and nights, knowledge of which would be more useful in characterising groups. Nevertheless, we found some marked differences among homeless people screened in the three types of venue.
Findings from analysis of screening locations
· The highest proportion of women was found in public places.
· The people screened in public places included those most recently turned homeless.
· The proportion of those born in Budapest was highest.
· People there relied least on the support of some organisation.
· Those screened in hostels felt the least healthy and complained the most about various diseases.
· They had the least proportion of people soliciting assistance from individuals.
· Those screened in daytime facilities included those who had been homeless longest.
· They had the highest proportion of people who approach some organisation for assistance.
· They declared themselves to be the most healthy, but yielded the highest rate of TB infection.
Sick (TB) as against healthy homeless people
· They spent more time on the Street and had been homeless longer (on average 51 months).
· They were older (average 48).
· One-fifth of them had already been treated for TB (17%)
· They were in a worse state of health (25% also complained of other diseases).
· They attended daily facilities in greater numbers (screening rate 4%).
Interviews with tuberculosis patients
As already mentioned, longer and more detailed questionnaires were completed for the 78 homeless people suffering from tuberculosis. This chapter presents the findings from these.
The questionnaire was made up of three parts:
1. The respondents' demographic and sociological details: educational level, father's educational level, occupation, marital status, number of children, etc.
2. Questions about the respondents' everyday homeless life: sleeping habits, sources of living, reasons for becoming homeless.
3. Determination of respondents' set of relationships, using eight "name-generation" situations43: could the respondent turn to anybody if he had personal problems, if he required medicines or health care, if he needed advice or money, was there anybody who let him do his washing, sleep occasionally, or looked after his possessions, and was there anybody to whom he could give help.
Demographic data
Detailed analysis confirmed the basic hypothesis that homeless people suffering from tuberculosis form a particularly disadvantaged groups within the homeless population as a whole: they are independent, solitary men, around 50 years old, out of work and have been homeless for a long time.
94 per cent of the 78 homeless TB patients were men, of average age 47. Nearly one in two (46%) were born in Budapest. 12% had been brought up in care. One in five - twice the average - had been in prison. As regards educational level, 37 per cent had completed 8 years or less of primary school, and 50 per cent were skilled workers. The figures for marital status and number of children bear out the solitariness of these 'people: 91 per cent were single or divorced, and 45 per cent had no children.
Distribution by place of birth
Table 1
 | % |
| Budapest | 46 |
| Other towns | 30 |
| Villages | 20 |
| Abroad | 4 |
Distribution by age
Table 2
20-29 | 30-39 | 40-49 | 50-59 | Over 60 | Total |
3 | 12 | 33 | 17 | 9 | 74 |
4% | 16% | 45% | 23% | 12% | 100% |
Distribution by level of education
Table 3
 | % |
| Less than 8 years elementary | 10 |
| 8 years elementary | 27 |
| Skills training secondary | 50 |
| Secondary | 13 |
The results concerning level of education are similar to those of the earlier studies: whereas the proportion of skilled workers in the Hungarian population is about 15 per cent, that of homeless people is at least twice as high, and in our case three times as high.
Proportion of skilled workers
Population, 1992 14.8%
Budaörs hostel, 199144 35,1%
Homeless people's hostels 199245 27,7%
Isola hostel 1993-9446 39,5%
Homeless people's hostels 199447 25,4%
Respondents’ fathers’ occupation (%)
Table 4
 | Respondent's
occupation | Respondent's father 's
occupation |
| Agricultural worker | 4 | 18.5 |
| Labourer | 16 | 21.5 |
| Semi-skilled worker | 18 | 3 |
| Skilled worker | 56 | 45 |
| Office worker | 1.5 | 1 |
| Mid-level white-collar | 1.5 | 3 |
| Management and intellectual | - | 3 |
| Other | 3 | 5 |
The observations of the Mezei-Sarlós investigation show that the occupation of 40.1 of skilled manual-worker homeless people is in the construction category, 25 per cent metallurgy, 11.6 per cent services, 20.4 per cent other, and 2.9 per cent agricultural48.
Looking at occupational category, skilled workers are overrepresented among homeless people. Around one-quarter are first-generation industrial workers: the fathers of 23 per cent of skilled-trade homeless people were agricultural workers.
In the younger age groups, similarly to other studies, we found a high proportion of those with at most 8 years of primary education and many with a background of childhood in state care.
Distribution by marital status
Table 5
 | % |
| Married | 8 |
| Divorced | 43 |
| Single | 49 |
Studies made amongst homeless people all agree that most homeless people are divorced or single people.
How many children do you have?
Table 6
 | % |
| No children | 45 |
| 1 child | 26 |
| 2 or more children | 29 |
Time of becoming homeless, by sex
Table 7
<6months | < 1 year | 2 years | 3 years | 4 years | > 5 years | Total |
3
4% | 7
9,5% | 14
19% | 10
13,5% | 12
16% | 28
38% | 74
100% |
Homeless people suffering from tuberculosis had spent longer on the streets than other homeless people: 54 per cent of them four years or longer.
Percentage distribution of homeless TB sufferers' sources of income (N = 78)
Table 8
 | % |
| Occasional work | 33 |
| Social benefits | 11 |
| Begging | 11 |
| Rental of own property | 8 |
| Collecting bottles | 8 |
| Dustbin-raking | 9 |
| Unemployment benefit | 4 |
| Disablement pension | 4 |
| Sale of collected items | 4 |
| Collecting paper | 3 |
| Old-age pension | 3 |
| Permanent employment | 2 |
None of the respondents, as a natural consequence of their condition, had permanent jobs. On average, their employment had ceased in 1989 (Std. Dev. 4.35), i.e. before the change of system.
19 per cent of the respondents had no earning or income, 50 per cent had one source of income, and most of the rest had two or three ways by which they made their living.
The average "income" of 29 per cent of respondents was 11,450 Ft (Std. Dev. 5,979). Table 8 shows that more than one-third of incomes is derived from occasional work. This is followed by begging and various benefits.
Occasional work was engaged in frequently by 41.5 per cent of the people questioned on the Street by the Mezei-Sarlós study, 21.2 attempted begging, but begging was accompanied, in 2.5 per cent of cases each, by collection of waste materials and occasional work. 19.3 per cent of respondents lived from social security benefits, 12 per cent from social benefits, 4 per cent from unemployment benefit, and 2.5 per cent from permanent work. The study found that 10 per cent of homeless people exist without receiving any money at all.
Percentage distribution of reasons for becoming homeless
Table 9
 | Total (N=78) | < 1 year homeless (N=10) |
| Family conflict | 40 | 34 |
| Discharge from workers' hostel | 25 | 26 |
| Divorce | 11 | 0 |
| Eviction | 10 | 8 |
| Discharge from other hospital ward | 3 | 0 |
| Withdrawal of service fiat | 3 | 8 |
| Ejected from own property | 3 | 8 |
| Released from prison | 2 | 8 |
| End of state child care | 1 | 0 |
| Home uninhabitable | 1 | 8 |
| Settled into homeless life | 1 | 0 |
As well as structural reasons (such as rising unemployment), it seems that it is personal reasons and conflicts that lie behind certain people (or groups of people) becoming homeless.
A large proportion of homeless men also said that they had ended up on the street because of the closure of workers' hostels, because their restricted financial means were insufficient to provide them with similar accommodation. The newly homeless, those becoming so within the preceding year, cited accommodation problems in greater proportions: for example, they could not afford the upkeep, repair or maintenance of their homes. (13 per cent of the sample had become homeless within the preceding year, and 60 per cent of them were born in Budapest.)
The immediate reason for becoming homeless in different studies (%)
(Reasons given by homeless people - one person could cite more than one.)
Table 10
 | 1991 Homeless persons' hostels (Gyuris - D.Molnár – Szántó) | 1994. Homeless persons' hostels (DMolnár) |
| Family and personal conflicts | 40 | 35,6 |
| Divorce | 29,2 | 20,8 |
| "Loss of contact" | 69,2 | 56,4 |
| Eviction | 8,3 | 7,6 |
| Home uninhabitable |  | 3,0 |
| Ejected from own home | 20,4 | 13,5 |
| "Loss of ownership" | 28,7 | 24,1 |
| Withdrawal of service fiat | 3,1 | 1,7 |
| End of workers' hostel place | 9,7 | 6,1 |
| "Unemployment homelessness" | 12,8 | 7,8 |
| Left institutions |  |  |
| Old people's home | 1,5 | 1,1 |
| Hospital wards | 4,2 | 2,5 |
| Psychiatric ward | 4,0 | 2,1 |
| Prison | 5,9 | 5,2 |
| State child care | 13,9 | 5,6 |
| "Institutional homelessness" | 29,5 | 16,5 |
| Chose "living tough" lifestyle | 5,1 | 4,2 |
Sleeping locations49
Table11
| Sleeping location | Total (N=64) | Only sleep in one place (N=26) | Sleep in differen places (N=38) |
| Some house or flat50 | 16 | 26 | 23 |
| Place in house as favour | 13 | 4 | 12 |
| Homeless persons' hostel | 32 | 54 | 42 |
| Empty building or cellar | 11 | 8 | 7 |
| Railway station | 14 |  | 6 |
| Public place/open air | 14 | 8 | 10 |
The sleeping habits of respondents were distributed relatively evenly among different locations. Only 32 per cent of the sample slept regularly in hostels. Those in the "unhealthy" group, however, were predominantly people who slept in night shelters.
It is clear from table 11 that those mentioning only one accustomed sleeping place were most likely (54 per cent) to spend their nights in some homeless people's or temporary hostel.
Of those who slept in more than one place, there were many more who were allowed as a favour to stay in a fiat, and those who lived on the street, in stations and in public places. These people moved around from day to day. The majority of this group were people who are probably incapable of organised or any other kind of coexistence in the long term.
Homeless TB sufferers' relationships with persons and institutions
We attempted to determine respondents' relationships with other people and with institutions serving the homeless, using the eight name-generator situations mentioned at the beginning of the chapter. It was already more or less apparent from the brief questionnaire that a large proportion of the homeless people were solitary people without relationships. Among those with tuberculosis, 36 per cent mentioned neither personal nor institutional contacts, and 28 per cent had one or more personal relationship.
Homeless people claimed only to turn to an institution for assistance at the last moment: 60 per cent of serious, hospitalised patients would approach an institution if they were sick and needed medicines or medical attention. Money was borrowed from institutions by 13 per cent of respondents.
Most respondents (14) approached other persons for advice (14 respondents). Only 5 were able to give any assistance. The average network size51 was 2 (Std. Dev. 1 .48), and the average complete network size52 was 3.5 (Std. Dev. 2.22). The "multiplexity index"53 which measures the closeness of relationships, was 2.2 (Std. Dev. 1.62). This number indicates very close personal relationships fulfilling several functions: the few people on whom homeless people can rely provide assistance in several different areas. (For comparison: in the network research carried out in 1987 by Róbert Angelusz and Róbert Tardos on a national representative sample, the average network size was 6.1 and the multiplexity was 1.2. Those without any relationships made up 1.6 per cent of the sample. The name-generator situations naturally differed somewhat from those used in our research.)
It was mentioned at the beginning of this chapter that the name, age, relationship with respondent, address and length of acquaintance of the persons mentioned by respondents were also recorded. The relationships were not homogeneous with respect to sex: the proportion of women among the 22 people questioned was 4.5 per cent compared to 38 per cent of people mentioned. Men often turn to female acquaintances for assistance. Because family relationships had broken down, respondents mainly relied on people out-side their families. (It is interesting that significantly fewer of those who mentioned family conflict as a reason for becoming homeless could rely on anybody. There was a significant correlation, R2 = .33, p = .003, between the network size and the family-conflict cause.) One-quarter of their relationships were social workers, and 20 per cent each friends and acquaintances. From families, reliance was chiefly on relatives (10 per cent), followed by parents and spouses (5% each). Other relationships (15%) were, for example, former prison cellmates, and doctors. Homeless people know each other and in certain cases also lend each other assistance. Nearly one-fifth of these relationships were themselves homeless people. Nearly three-quarters of the non-homeless people lived in Budapest, and so were physically close and could be relied on. Half of relationships were of several years' standing, and the other half very new. This is not surprising, considering that the respondents had been contacted by social workers only shortly before, and had got into closer relationship with them mainly in connection with some illness.
Chapters 3 and 4 contain some findings which are completely new, and not analysed elsewhere. We hope that in the near future, both in further screening and in other research among homeless people, we will have more comparative data, and will thus get closer to an answer to the "big question": Who are becoming homeless in Hungary now, and why exactly them?
Concluding remarks
Standing up for the interests of homeless people, or other people on the periphery, is not a straightforward task. It becomes especially hard if the matter touches on a range of different areas which are all themselves under-financed. Many can see the problem, but few make serious efforts to address it. The responsibility, when it comes to action, always lies with "the other side". The basic reason for this is plain enough: the sad truth is that the poorest and defenceless are not really important to anybody.
This programme was successful nonetheless.
If were to examine the reasons for this with a jaundiced eye, we might venture the explanation that the poor man's tuberculosis is more of a threat than his toothache, fever or ulcer. Everybody can get TB, and this makes it a public matter.
But perhaps there is an aspect of greater moment. Something very simple, and increasingly rare in the modern world: cooperation.
The outline: the Budapest City Council notices, recognises, and tries to solve the trouble. And fails. The Soros Foundation takes note, and sets up a grant scheme. The applications are not judged individually, but -surprisingly - the applicants take up the task collectively, each doing what they are best at.
Then come two very hard years before a solution is found to the problems of how to contact homeless people, for one occasion to be enough to take and interpret the X-ray, for social workers to work together on the streets with doctors and health care staff, for hospitals to accept the patients, and for social workers - in lieu of relatives - to visit and provide for patients. Convalescent facilities are arranged in place of a home and to assure complete recovery of people with no home of their own. Ministerial finance arrives.
Putting it more simply: the state (the Ministry and the Budapest City Council) detect the trouble but are unable to resolve it. The civil sphere steps in as a catalyst, setting up and testing a model. The state reappears, and re-assumes, or at least finances, the action. This is a model. A model of how a civil society can operate, how tasks within it can be assigned.
Unfortunately, some things are still lacking.
The bus is ready to go, but does not operate for six days of the week. Not because there are no homeless people on the streets, but because there are no empty beds in the hospitals. One feels thwarted. 20-30 new hospital beds are needed, and perhaps the same number of convalescent beds. It would also be welcome if somebody (the Ministry of Welfare? Budapest City?) would take over the expenses of hospital social work from the Soros Foundation. It would also be good if the running of the bus, instead of having to rely on uncertain ministerial support, which has tó be fought for on every occasion, was met through a contract with the National Health Insurance Fund.
And best of all would be if in a few years time, the screening equipment could be removed from the bus and replaced by seats to take children on trips, because there were no more people with tuberculosis, or, indeed, people without homes.
Budapest, May 1997.
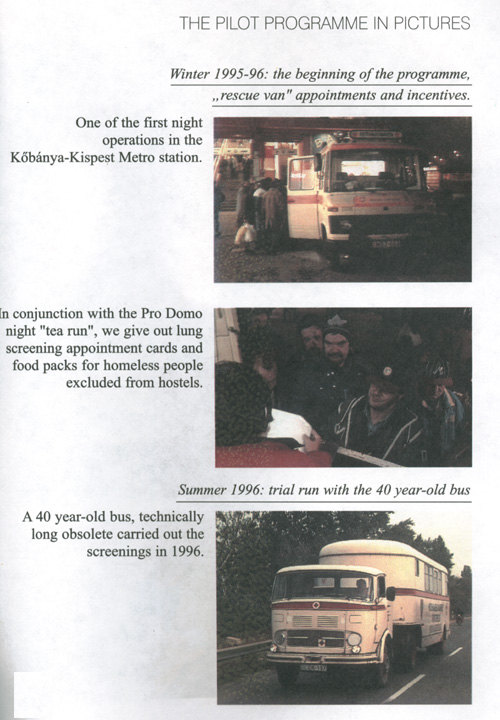
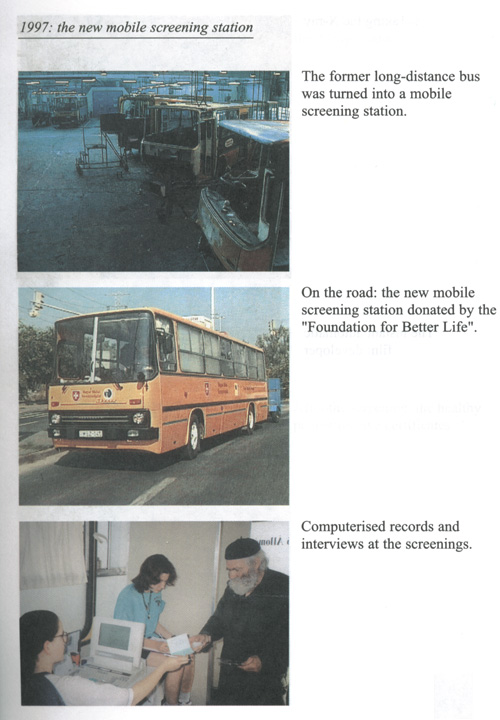
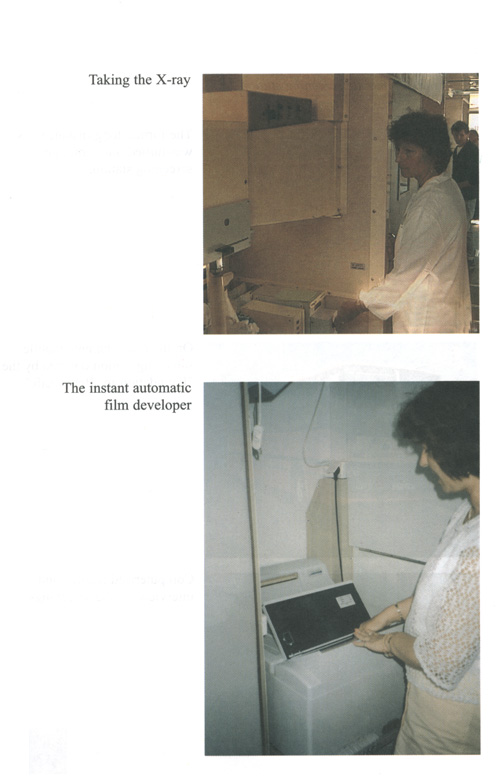
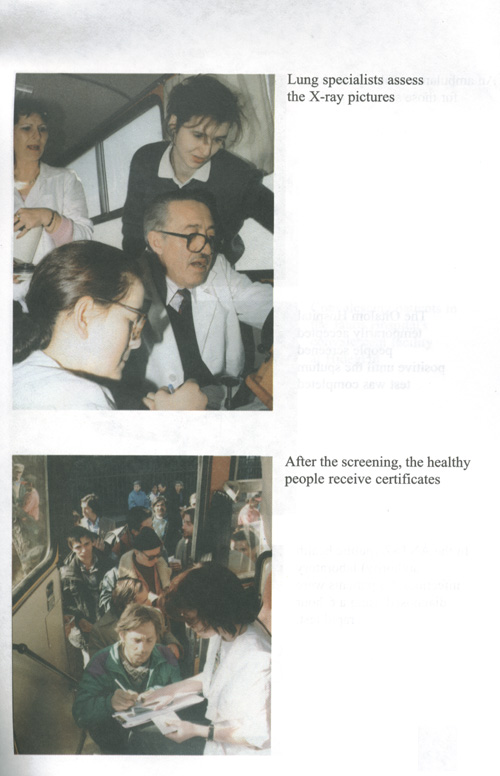
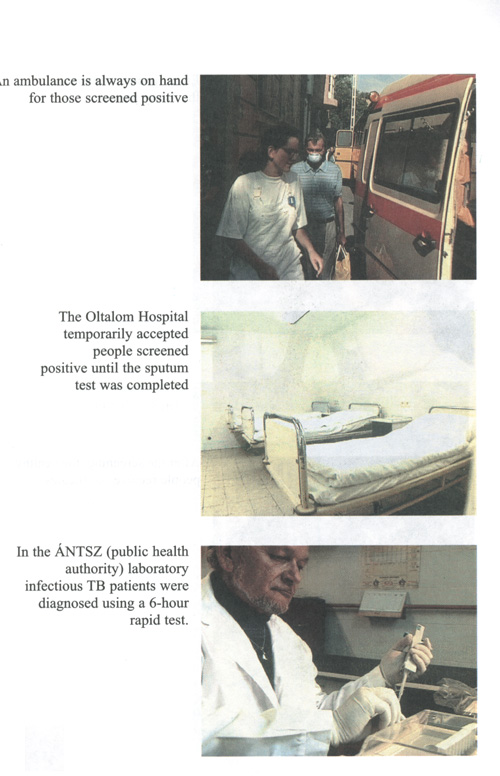
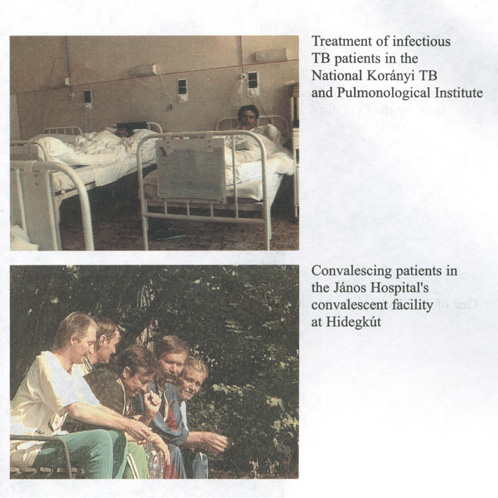
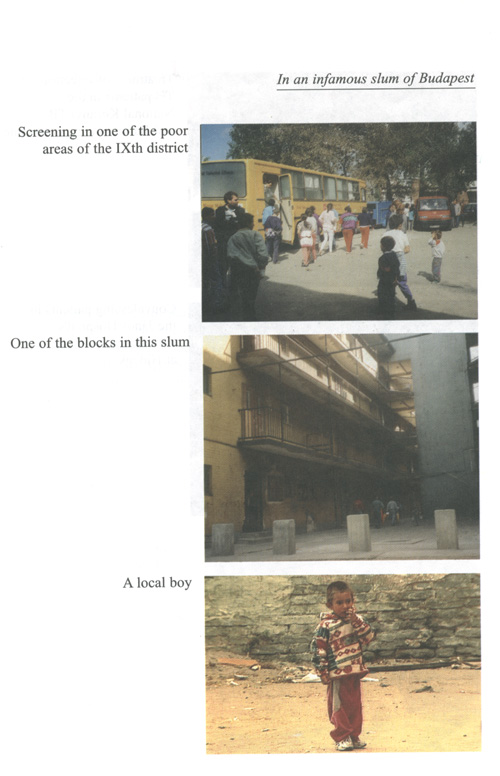
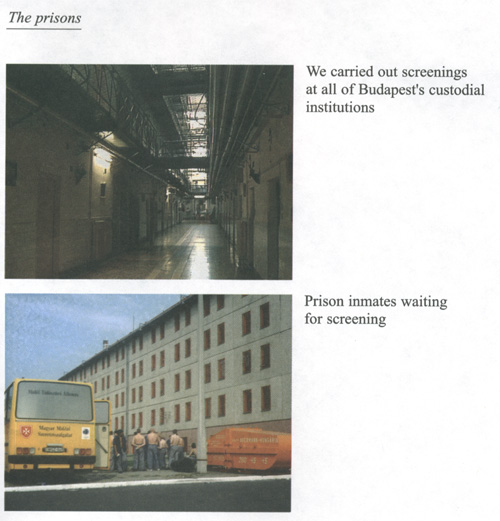
1 László Levendel: The homeless person. OAI, 1993.116 pp
2Sources: Hungarian Statistical Yearbook 1992, CSO, 1993, Hungarian Statistical Yearbook 1995, CSO, 1996; László Levendel: The urgency of social rehabilitation of deprived TB patients. in: Tovább... Papers by László Levendel. OAI, 1994; Dr. Erzsébet Ábrahám, D. László Karácsonyi, Dr. Elek Dinya: Could tuberculosis become widespread again in Hungary? (Model investigation, 1968-1993) in: Orvosi Hetilap (Medical Weekly), 18 June 1995; Dr. Imre Vadász, Dr Zsuzsa Popovics, Dr. Tamás Fodor: Who is dying of tuberculosis in the 1990s? in: Orvosi Hetilap, 17 October 1993; Dr. Ottó Schweiger: The changed face of tuberculosis. Népegészségügy (Public Health) no. 2, 1995; Dr Ottó Schweiger: Tuberculosis. in: Forum Pulmonologicum, no. 9; Árpád Pünkösdi: Dr. Koch's little sticks (Népszabadság, 1 July 1996); Interview with Dr Zoltán Ajkay (Népszabadság, 26 Deptember 1996); Júlia Gáti: Tuberculosis strikes again. The disease of the poor. HVG, 6 April 1996
3 incidence = number of new patients registered in one year
4 Hungarian Statistical Yearbook 1995, CSO, 1996
5 Hungarian Statistical Yearbook 1995, CSO, 1996
6 Dr. Ottó Schweiger: The changing face of tuberculosis. Népegészségügy (Public Health), no. 2, 1995.
7 László Levendel: Urgency of rehabilitating deprived tuberculosis patients. In: Tovább... Papers by László Levendel, p 33, OAI, and the Hungarian Statistical Yearbook 1995, CSO, 1996.
8 The 1995 data were provided by Dr Dezső Kozma.
9 Dr. Ottó Schweiger: The changing face of tuberculosis. Népegészségügy (Public Health) 1995, no. 2
10 Dr. Erzsébet Ábrahám, Dr. László Karácsonyi, Dr. Elek Dinya: Could tuberculosis become widespread again in Hungary? (Model investigation 1968-93). in: Orvosi Hetilap (Medical Weekly), 18 June 1995.
11 Interview with Dr. Katalin Heylmann, Health Director of the National Penal Enforcement Authority and Dr. Mihály Németh, public health consultant HÁLÓ January 1997, p 12-13
12 At the request of the Health Director of the National Penal Enforcement Authority, our programme carried out, between 22 July and 7 August 1997, screening of all persons held in Budapest penal institutions. This amounted to 1969 screenings. Of these, 39 persons were referred for further examination. Further examination and treatment is being carried out by the Tököl Prison Hospital.
13 The results published in the book are drawn from a medical-sociological survey carried out in Zala county in 1977-78. Ágnes Losonczi, Ártó-védő társadalom (The harmfully protecting society). Budapest, Közgazdasági és Jogikönyvkiadó, 1989.
14 Ágnes Bokor: Poverty in Hungary today. Magvető, 1987, 169 pp
15 Dr. Imre Vadász, Dr. Zsuzsa Popovics, Dr. Tamás Fodor: Who are dying of tuberculosis in the 1990s? in: Orvosi Hetilap (Medical Weekly), 17 October 1993.
16 Dr. Katalin Gál: Homeless TB sufferers in the Budapest health care system. MS, 1994
17 For literature related to the homeless people's state of health see: Hajléktalanság sebei (Wounds of homelessness), eds Klára László and Jolán Oross, In: Periféria Seria 6, NM, 1996
18 See: Jolán Oross: Itthontalanul (Without a home), OAI, 1992.
19 See: Dr. László D. Molnár and Dr. Klára László: State of health of the homeless in Budapest. In: Hajléktalanság sebei (Wounds of homelessness), Periféria Seria 6, NM, 1996
20 See: 1995 Report on Budapest Social Services Centre and Institutes
21 György Mezei: Az álmok kapujában (At the gateway of dreams). Periféria Füzetek 96/3.
22 The significance of the cigarette in the lives of homeless people goes further than a smokable rod of tobacco. It is a means of barter, with a value far above its price, just as it was among front-line soldiers in times past, and indeed it is a mark of status for somebody within the community to have cigarettes to offer.
23 Summary by Dr. Dezső Kozma.
24 The Oltalom Charity Society also operates a general practice surgery and a crisis ward "mini-hospital" for homeless people.
25 Dr. Zoltán Ajkay some time ago urged screening of homeless people by a new method, centred on collaboration between civil organisations and on convalescent care.
26 Dr. Anna Ungár carried out pioneering work in detecting homeless tuberculosis sufferers with whom lung specialists had lost contact with, and it was via this that some lung specialists first established widespread contacts with institutions serving home less people.
27 The screening interview was taken by several social workers. The data was processed using the SPSS computer program. Data for a total of 2998 people was processed. The interview questions were: Name of interviewer, place and date of interview. Details of interviewee: name, mother's maiden name, date and place of birth, usual place of residence or accommodation. How long have you been homeless? Who do you receive assistance from? (In the first column were listed various institutions for the homeless, in the second column people - parent, spouse, child, relative, friend, colleague, acquaintance, social worker, other). Do you have a regular income? Do you have a social security (health service) card? When did you last attend a lung screening: What was the result? Have you ever been treated for TB infection? Are you being treated now? Do you have any other diseases? When did you last visit a doctor? Do you fell healthy? Do you have a fever? Have you lost weight? Do you smoke? If so, for how many years? Do you drink alcohol every day? If yes, what kind - spirits, beer, wine?
28 György Mezei and colleagues questioned 457 homeless people in 1992 and 1993, in Budapest railway stations, Deák Square and at various soup-kitchens. Their other sample was drawn from the Isola night shelter, where 122 homeless people were inter- viewed using the questionnaire also used on the streets. The total number of people using the 80-bed refugee in the period of the survey was 723. Katalin Sarlós and György Mezei: Nyomorskála (A Scale of Poverty). Terem a Nyomor Füzetek (Fruits of poverty series) 1, 1995.
29 The control-sample research carried out by SzocioMed Kft in 1994 on the state of health of Budapest homeless people in hostels, on the streets and in hospitals. The sample consisted of 342 homeless people. Dr. László D. Molnár and Dr. Klára László: The state of health of the Budapest homeless. In: Wounds of homelessness. Periferia Seria 6.
30 The major surveys of homeless people, and mainly carried out in hostels, were the following, in chronological order. The first large survey (160 people) was made in 1991 in the biggest homeless people's hostel in Budaörs. (Jolán Oross: Itthontalanul OAI, 1992) in 1991, a survey carried out using the computer information system operated by the Intel Comp Foundation and financed by the Ministry of Welfare, 545 homeless people in 2 Budapest hostels and 11 hostels elsewhere were interviewed on the basis of a questionnaire, the data being processed by Tamás Gyuris, László D. Molnár and Róbert Szántó. (Tamás Gyuris, László D. Molnár, Róbert Szántó: Hajléktalanok -Homeless people - Periferia Füzetek 95/4.) in 1993 and 1994, the Pro Domo Peripheral Groups Methodology Group investigated hostel registration book data ön 8998 residents of 3 homeless persons' hostels in 45 towns and villages. (Mihály B. Kocsis: Magyarország menhelyei - Hungary's refuges - Periferia Seria 4. NM, 1995). An investigation was carried out by Zoltán Gurály on clients not of hostels, but of offices serving homeless people, involving 5852 homeless people. (Zoltán Gurály: Az utcán - On the Street -1990-95, MS, 1996).
31 Those who came to the first screening having been treated at some pulmonary care centre, and could certify that they had attended within the last month, only had to complete the questionnaire. Those lacking such certification were some of the people who only filled the questionnaire, or perhaps even went to the screening but did not return. Unfortunately it often happened that it was just those who were screened positive that did not return.
32 130 people were referred from the screening programme for further examination. 92 of these provided data for this sample.
33 Proportions of women in various studies: Mezei-Sarlós 11%, D. Molnár-Gyuris-Szántó 15.8%, Oross 11%. The low proportion of women may be due to women having more opportunities for securing a place in somebody's house as a favour, and for younger women from acquaintances or occasional partners, so that they are less likely to end up on the Street or in refuges. This is supported by the fact that twice as many women (28%) than men indicated the "other" place-or-residence category, which consists mainly of private flats, caves, tents, etc. A similar conclusion can be arrived at from the Street survey carried out by the Pro Domo Peripheral Group Methodology Department carried out among homeless people in winter 1995 (207 people). Responses to the question, "Where did you sleep last night?" showed that men spent the night in refuges much more often than women, and women more often in public places or with acquaintances or relatives. Of all respondents (143 men and 38 women), 8.3 per cent had spent the preceding night at an acquaintance or relative. For men this was only 4.2 per cent, and for women, 23.7 per cent. It is also true, however, that 70% of the places providing accommodation for homeless people across the country only accept men. This could also explain some cases of women's "other" accommodation strategies.
34 Hungarian Statistical Yearbook 1995, CSO, 1996
35 From our own two questionnaires.
36 Hungarian Statistical Yearbook 1995, Mezei-Sarlós 1995, D. Molnár 1995.
37 Of the studies carried out in recent years, two produced different results from those presented so far in respect of age distribution. One was the 1994 Pro Domo study carried out in 95 per cent of the homeless people's hostels then in operation (Kocsis, 1995). The age distribution of the 7346 residents (1489 women, 5291 men) showed that 20 per cent of men and 46 per cent of women were under 30, and that those between 31 and 60 constituted three-quarters of men but only half of women. The other survey (Gurály, 1996), involving 3108 homeless people among the clients of the Menhely Alapítvány (Refuge Foundation) between 1990 and 1995, found that home less women are predominantly younger and men older, but still within the active age groups.
38 It is of course possible that, since the place of origin was not asked, this figure includes those born in Budapest hospitals.
39 Budapest Statistical Yearbook 1995, p 89 Total permanent and temporary immigration.
40 Hungarian Statistical Yearbook 1995, p 59
41 The question "since when have you been homeless?" was not answered by 3.6% of those questioned, and they gave their place of residence as "other". In these cases this mainly meant private flats, which especially for women does not exclude beyond doubt that they were in fact homeless. In many cases the private fiat address indicates use of the fiat as a favour.
42 These numbers are only indicative. Since we did not record each year, but calculated using the arithmetic mean of the interval, the results are not very precise.
43 Using the "Fischer method" often mentioned in the network literature, we attempted to cover the person's entire set of relationships. We devised eight situations, in each of which we asked if the respondent knew a person or persons to whom he could turn to for help in the given situation. For each of the persons thus mentioned, we recorded their name, age, relationship with respondent, educational level, and address. In two of the situations we also asked the respondents’ institutional relations: where they could approach in case of illness.
44 Jolán Oross: Itthontalanul (Without a home). OAI, 1992
45 Tamás Gyuris, László D. Molnár, Róbert Szántó: Homeless people. Család, gyermek, ifjúság (Family, children and youth), 1992/1-2.
46 György Mezei and Katalin Sarlós: Nyomorskála (Scale of Poverty). Terem a nyomor Füzetek 95/4.
47 László D. Molnár: Hajléktalanok (Homeless people). Periféria Füzetek 95/4.
48 György Mezei and Katalin Sarlós: Nyomorskála
49 The question on the questionnaire was: Where have you spent the night in the last year? More than one answer could be given.
50 Here we merged the following categories: own home, squat, temporary home, service fiat, sub-tenancy, bed-only tenancy, IBUSZ hostel room.
51 The number of different people mentioned by respondents.
52 The total number of persons mentioned.
53 The multiplexity index is the ratio of the complete network size and the network size. If the multiplexity index is 1, then each relationship has a single function. The higher he number, the more functions are met by the same relationships.